More than half a million women had some form of cosmetic breast surgery in 2017—be it an augmentation, a lift or a reduction—according to the American Society for Aesthetic Plastic Surgery (ASAPS). Breast augmentation—improving the size and shape of the breasts with implants—is the most popular plastic surgery procedure year after year. Lifts, which elevate sagging breasts to a more pert position, saw a 57.5 percent jump between 2012 and 2017. Breast reduction surgery continues to gain steam, as well, establishing itself as far more than an aesthetic fix, but a total women’s-health solution—a pain-relieving, life-altering procedure for patients of all ages. Each procedure is tailored to address your personal concerns and suit your body and lifestyle. Here, a comprehensive look at breast surgeries of every kind.
You May Also Like: 5 Things To Know Before Getting Breast Implants
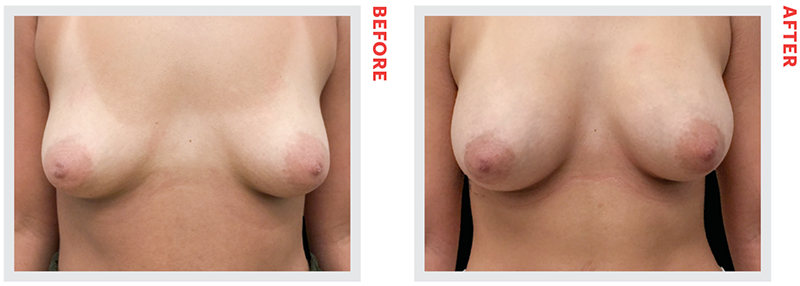
New York plastic surgeon Craig A. Baldenhofer, MD used an inframammary approach to place 325-cc Mentor smooth, round, silicone implants, which gave this 24-year-old patient the larger cup size she desired.
Breast Augmentation
Whether you were born with small breasts, or yours simply shrunk from pregnancy or age, a breast augmentation can enhance or restore curves (and bolster confidence, too: Imagine finally filling out that bikini top, or effortlessly holding up a strapless dress). Average treatment cost $3,500– $10,000
Decisions, Decisions: Implant Selection and Placement
“Making good decisions on the front end can help produce great outcomes with the lowest risk of reoperation or complications,” says Eugene, OR plastic surgeon Mark Jewell, MD. Read on for everything you need to know.
Size
As a general rule of thumb, every 200 cubic centimeters (ccs) of volume will boost you up about a cup. Your unique size and shape will steer you to the right range. “The base width of your chest is going to define the parameter of implants we can safely choose from,” says New York plastic surgeon Umbareen Mahmood, MD. What’s more, your skin may impose a size limit “if there’s a tight envelope to the breast tissue,” says Dr. Jewell. Even if it doesn’t, prudent doctors urge patients to consider how their implants of choice will age with them. “Be cautious: The bigger the implants, the more the skin may stretch over time,” says Dr. Mahmood. Beyond drooping, “large, heavy implants can lead to the same complications as large breasts—back, neck and shoulder pain, shoulder grooving from bra straps, and difficulty exercising,” warns New York plastic surgeon Melissa Doft, MD.
Profile
The base diameter of the breast also determines how wide of an implant can be used. “For two women who wish to have the same size, one with a narrow chest will typically need a higher profile implant than one with a wider chest,” explains Dr. Doft. But most patients do well with a moderate profile. “For women lacking projection due to massive weight loss or breast deflation following nursing, a higher profile may be needed to fill out the missing space,” says San Francisco plastic surgeon Karen Horton, MD.
Fill
The majority of patients and surgeons prefer silicone-gel implants to saline (salt water– filled), citing a more natural look and feel. (And it’s worth noting: “Silicone breast implants are the most widely studied medical devices in the history of medical devices,” says Dr. Horton.) The newest kinds are “form-stable, so if they tear or ‘rupture,’ the silicone doesn’t leak out and the implants maintain their shape,” adds Dr. Doft. According to Santa Monica, CA plastic surgeon Steven Teitelbaum, MD, silicone implants are also lighter and less apt to bottom out and stretch the skin. With saline implants, “their contents slosh up and push down on the skin repeatedly, day by day,” he says. This so-called “water-hammer effect” may cause a greater degree of droop over time. Saline implants are also more prone to rippling (a problem for thin women, in particular) and don’t lend much fullness to the upper breast (hence, poor cleavage). “The main benefit of saline is that you have immediate detection of rupture,” says Dr. Mahmood. The implant deflates and saline is harmlessly absorbed by the body. They also tend to be less costly and may require shorter incisions because their shells are filled only once inside the body.
Shape
Implants can be round or teardrop-shaped. Round, silicone implants now come in various gel configurations, says Dr. Jewell, each designed to deliver more fullness or “pop” to different aspects of the breast. Shaped implants “have a tapered upper edge and give the most projection behind the nipple-areola for an anatomic look, and can be good for women who don’t have much breast tissue to begin with,” he adds. They may also benefit those with chest wall depressions and asymmetries, in addition to patients “whose breasts have constricted lower poles, as they tend to give better expansion at the bottom part of the breast,” Dallas plastic surgeon William P. Adams Jr., MD explains. Shaped implants have two big drawbacks, however: they can rotate out of position, creating an obvious asymmetry that requires surgery to correct; and they all come with textured shells (roughed up to better grip the breast tissue), which have been linked to breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). This is a rare and treatable type of T-cell lymphoma that can develop around breast implants, which is theoretically due to bacterial contamination during surgery. “For women needing contour, but wanting to avoid textured shells, smooth, firm ‘gummy bear’ implants may be an alternative,” says Dr. Horton. “They’re often used in breast cancer reconstruction because they hold their shape so well.”
Shell
An implant shell can be smooth or textured. Smooth implants, which have long been more popular in the U.S., “glide and slide naturally in the pocket, or space around the implant, whereas textured ones, with their Velcro-like shells, can create a stiffer, more immobile result,” according to Dr. Horton. Due to the association between textured shells and BIA-ALCL, many surgeons now offer smooth exclusively.
Incision
Surgeons can place implants through incisions in the fold beneath the breast (the inframammary approach), in the bottom curve of the nipple (periareolar), or in the armpit (transaxillary). “Underneath the breast is probably the most favored, as it gives the best visualization of tissue and the greatest precision, and allows you to adjust the fold up or down,” says Dr. Jewell. Plus, this incision is well hidden. “And because the breast gland is not dissected [as it is during periareolar placement], there’s no potential injury that could affect breastfeeding in the future,” adds Dr. Doft. (Cutting through the breast tissue can also introduce bacteria from the milk ducts into the surgical field, hiking the risk of infection and complications.) “The armpit approach tends to beget “a bigger and less-precise operation,” notes Dr. Jewell.
Placement
Three options: Submuscular involves creating a pocket for the implant behind the pectoralis muscle, which then covers it either fully or partially (dual-plane is the term for this—the top of the implant is covered by muscle, the bottom by soft tissue); subfascial means inserting the implant beneath the fascia, or mesh-like connective tissue overlying the muscle; and subglandular, or placing the implant over the muscle and beneath the breast tissue. Dr. Adams says, “If you add up all the checks and minuses, I think submuscular/dual-plane is the safest option because there’s muscle between the breast tissue and the implant, providing a barrier against potential bacteria.” (Subglandular carries a higher risk of capsular contracture.) Doctors also consider a patient’s build and lifestyle when determining placement: “I operate on many athletes who have little to no body fat and are concerned about their pec muscles being disrupted. So, while ordinarily my preference is to go dual-plane, I’ll go under the fascia for them, so as not to affect the muscle,” says Dr. Mahmood. Dr. Jewell also prefers subfascial placement for athletes with adequate breast tissue because “going behind the muscle can create what’s known as an animation deformity—the implants shift and breasts flatten out when the patient flexes her pectoralis muscles,” he explains.
What to Expect
An Educational Consult
“The more patients know about the augmentation process, the fewer LIFT surprises they face, and the better they do overall,” says Dr. Adams. Your surgeon will ask you about your goals and expectations, measure your breasts, guide you through implant selection, and discuss surgical strategy. Patients typically “try on” implant sizers as they would clothes, so they can see what works. Some also use 3-D imaging to approximate results. Your surgeon should review risks of breast augmentation, including capsular contraction (a thickening and tightening of the scar tissue that forms around implants), rupture and BIA-ALCL.
A Quick Outpatient Procedure
Breast augmentation takes one to two hours, and is done under general anesthesia. You should be able to return home the same day.
A Fairly Comfortable Recovery
When you awake from surgery, your incisions will be covered and your chest may be wrapped. Expect one to two weeks of bruising, swelling and discomfort. (Placing implants under the muscle generally results in more post-op pain, “because the muscle is being stretched and there are many pain fibers within the muscle,” says Dr. Horton.) Doctors recommend wearing a soft postoperative bra to lend comfort during healing (no underwires for several months). Any non-dissolvable stitches are removed after one to two weeks; drains come out within a week. (Some surgeons use drains to head off complications. As Dr. Horton explains, “Wound fluid is filled with proteins and sugars that can serve as a medium for bacterial growth. By gently whisking away this fluid as it forms, drains can minimize swelling, speed recovery and lessen the chance of capsular contracture.”) You’ll need to skip exercise for about three weeks. Breasts will gradually drop and settle: “It can take around three months for the implants to really feel like a part of you,” Dr. Horton says. Sensation usually recovers over a few weeks to months.
Living With Implants: Maintenance & Monitoring
How Long Will My Results Last?
While breast implants are not lifetime devices, modern models don’t have the predictable expiration date of implants past: “We used to say to replace them every 10 years, but now most doctors suggest swapping them out only when you have an issue,” says Dr. Doft. If you notice any change in the look or feel of your breasts, contact your surgeon right away.
What Sort Of Monitoring Will They Require?
The FDA recommends that women with silicone implants get MRI screenings to detect silent ruptures three years after surgery, and every other year after. (Saline ruptures are marked by obvious deflation, making MRIs unnecessary.) “It’s also important to check in with your plastic surgeon periodically to monitor your outcome,” says Dr. Jewell.
What Should I Watch For?
Capsular contracture, which can render breasts hard and distorted, is the most common complication. “It’s clearly mediated by bacteria, so we take steps to minimize the amount of bacteria around the implant, and these steps have been shown in multiple studies to be efficacious at reducing capsular contracture. Twenty-five years ago, the rate was up to 50 percent. Now, with our current techniques, it’s less than 2 percent,” says Dr. Adams. Another rare risk, BIA-ALCL can present as fluid around the implant, or as a lump in the breast or armpit. “It’s not the feared problem we thought it was a few years ago and data shows that when precautions are taken to prevent contamination, textured implants should be safe,” says Dr. Jewell. As of press time, it has been documented in 427 patients worldwide—all with textured implants—out of the approximately 20 million patients who have implants.
How Will My Results Age?
“The less breast tissue someone has, the fewer changes we tend to see over time,” says Dr. Adams. “People with a decent amount of breast tissue may experience more dynamic changes and have a higher chance of developing sagging, and at some point, needing a lift or tightening procedure.”
Will I Be Able to Breastfeed After an Augmentation?
“Our data shows that women with implants don’t have a higher incidence of lactation issues than those who don’t have implants. If someone who has successfully breastfed in the past has an augmentation, and then goes on to have another child or two, she’s usually very successful at nursing,” Dr. Jewell says.
How Do Implants Affect a Mammogram?
Women at average risk for breast cancer should follow the American Cancer Society’s screening guidelines—annual mammograms starting at age 45, and biannual at 55-plus— unless otherwise directed by their health-care provider. Because mammograms can’t see through implants, the technician will need to take additional scans “with the implants pushed back against the body and the breast tissue pulled forward onto the plates,” says Dr. Teitelbaum. Whether implants are over or under the muscle, “mammograms are still generally effective, as long as the implant is soft and the breast tissue is mobile,” he adds.
In the Pipeline
In a move to diminish complications, certain breast implant manufacturers are reengineering textured shells to make them less hospitable to bacteria. Currently in clinical trials, Motiva’s “nanotextured” implants are claiming low capsular contracture rates and thin capsules—the data looks encouraging. Implant-maker Allergan is reportedly contemplating a new, less-aggressive texture for its implants, as well. Aiming to sidestep breast strain and drooping, the B-Lite implant—said to be up to 30 percent lighter than traditional implants (and still in trials)—suspends tiny, hollow glass spheres in silicone gel. “The theory is that if you have a lighter-weight implant, you’ll have fewer problems with malposition, and that’s a great idea,” says Dr. Jewell. “On the other hand, what happens to all those microscopic glass beads if the implant ruptures? The long-term safety profile of the B-Lite remains to be determined.”
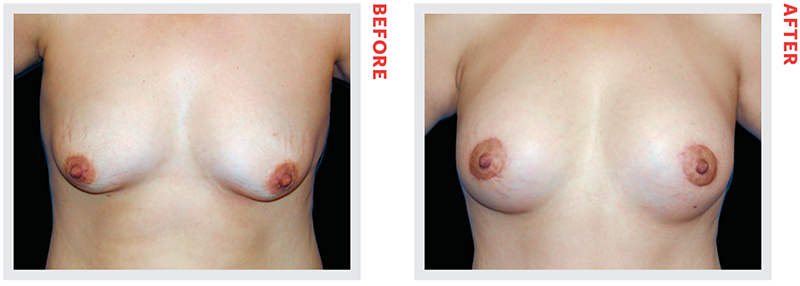
Unhappy with the way her breasts appeared after multiple pregnancies, this 42-year-old patient underwent a circle breast lift with implants, performed by Encino, CA plastic surgeon George Sanders, MD.
Breast Lift
A breast lift can repackage fallen breast tissue into a perkier shape. While some lift-seekers suffer from deflation plus laxity, and may need the added boost of fat or implants, “others have adequate volume, it’s just in the wrong place,” notes Dr. Jewell. Surgeons gauge the severity of droop (“ptosis”) by the position of the nipple: On a youthful breast, the nipple is at, or a bit above, the fold. “The distance the nipple descends, to ultimately pointing at the floor, the greater the ptosis,” says Dr. Mahmood. Average cost $4,000–$12,000
What You Need to Know
How long is the surgery?
Depending on the surgical approach used, it can take between two and four hours, says Austin, TX plastic surgeon Jennifer Walden, MD.
Will I need implants?
“When someone has a fair amount of breast tissue, the gland itself can provide necessary volume,” Dr. Walden says. That tissue can be used alone or combined with fat to create the desired fullness. But generally “when a patient is asking for actual cleavage—that nice upper-pole fullness—they really need the structure of an implant,” Dr. Mahmood notes.
What will my scar look like?
Doctors often reference a lollipop scar (a circle around the areola with a vertical line running down the middle of the breast) or an anchor scar (the lollipop configuration with a horizontal incision along the breast fold). “The circle helps to move the areola upward and decreases its diameter. The vertical incision—or lollipop stick, if you will—helps to tuck the skin inward, narrowing the width of the breast. But to achieve a significant lift upward, a horizontal vector is needed, too, and this falls in the breast fold,” Dr. Horton explains. By incorporating liposuction into a lift or reduction to “debulk the bra-roll region,” she’s often able to shorten that lower scar “so it doesn’t peek out from the sides of a bathing suit or bra.”
Will my breasts fall again?
When working with thin breast tissues, “our constant battle is trying to hold the results of the lift long-term,” says Dr. Walden. Lending support are new kinds of mesh scaffolding, like GalaFORM 3D, which can improve the longevity of lifts in select patients by serving as a sort of internal bra. But, because they can up the price of surgery by $1,500 to $3,000, they’re not a standard add-on.
How will I feel after surgery?
“For three weeks, you’re not lifting anything over 10 pounds—including children. Someone else has to be the primary caregiver during that time. And then no push-ups, pull-ups or intense yoga for six to eight weeks,” says Dr. Walden.
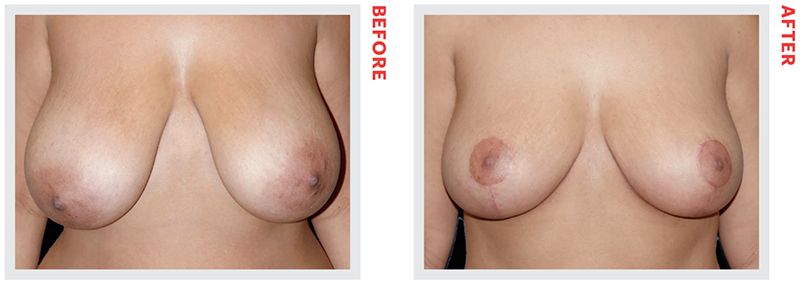
Scottsdale, AZ plastic surgeon Bryan W. Gawley, MD performed a breast reduction on this 35-year-old patient to alleviate the chronic shoulder and back pain caused by her heavy breasts.
Breast Reduction
Reductions focus on form—creating pretty, balanced breasts—and function, “alleviating neck, shoulder and back pain, as well as persistent rashes that form under the breasts,” says Dr. Jewell. A breast reduction can buoy self-esteem, enable women to work out more easily and even expand their wardrobe options. “A big part of the reduction is actually a major lift,” Dr. Horton notes. Surgeons use a number of techniques to debulk the bottom and sides of the breast, making patients at least one to two cup sizes smaller, before creating a perkier shape and moving breasts to a higher position. Average cost $12,000–$18,000
What You Need to Know
How long is surgery?
Three to four hours, on average
Will my breasts still be functional?
During reductions, surgeons create pedicles, or stalks of tissue, to add shape to the breast while supporting and nourishing the nipple throughout surgery. There are several different pedicle approaches, but many doctors favor the superomedial technique, which supplies blood from the upper part of the sternum, and is thought to “provide the perkiest upper pole, and preserve the best sensation, blood supply and ductal supply to the nipple,” according to Dr. Horton. Regardless of technique, “anytime we manipulate the tissues of the breast, lactation problems and changes in sensation are always possible,” says Dr. Walden.
Is it covered by insurance?
In many cases, yes, but there’s a catch: “The insurance company can then dictate, based on body surface area calculations, how much volume we take out, which can sometimes bring a patient down to an A cup,” says Dr. Mahmood. With a “custom reduction,” notes Dr. Jewell, “we can remove less tissue than what’s required for insurance coverage, and produce a very pretty outcome.”
How will I feel after surgery?
Tired! “Fatigue is the number-one symptom,” says Dr. Horton. “A breast reduction involves a large surface area, and the wounds can really sap your energy.” Her patients also report feeling very emotional during recovery, “like terrible PMS,” she says. Plan on taking two to three weeks off work (including primary parenting) and four to six weeks off aggressive exercise. “The fitter a woman is going into surgery, the smoother her recovery should be,” she adds.
Breast Reconstruction
Following a lumpectomy or mastectomy, breasts can be rebuilt—either restored to their previous proportions or reimagined to meet patients’ expectations— via three distinct means: “A tissue expander plus breast implants; flap/autologous reconstruction, which uses the patient’s own tissue, skin and fat from their stomach or back; or fat grafting,” says Jericho, NY plastic surgeon Kaveh Alizadeh, MD. Because not every patient is a candidate for the latter two methods, most reconstruction surgeries involve implants. According to Campbell, CA plastic surgeon Kamakshi R. Zeidler, MD, about 75 percent of women choose implants, and there are two ways to place them: “The traditional way is to place them in two stages, with temporary implants (balloon-like tissue expanders) that are later changed to permanent ones. The other option is to place the implant directly after removing the existing breast tissue in a single surgical procedure called direct-to-implant [DTI],” she says. “If the tissue is not significantly affected from the cancer removal, we may be able to place the implant directly.” The patient’s anatomy, how her mastectomy or lumpectomy was performed, and the type and severity of her cancer all play a role in the surgery.
A flap reconstruction “harvests tissue from the stomach or back to recreate the breasts, and can be very technically demanding, lengthy and complex— it also results in a more intense recovery,” says New York plastic surgeon Daniel Maman, MD. The upside: New breasts usually feel very natural, and come with none of the upkeep or potential complications associated with implants. While there are various types and subtypes of flaps— categorized by their origin and the degree of skin, fat, and/or muscle comprising them—“tissue flap reconstruction is generally reserved for more challenging cases that cannot be done with tissue expanders,” says Dr. Jewell.
Transferring fat to the breasts from the butt, belly, flanks or thighs via liposuction and subsequent injections can soften the contours of newly reconstructed breasts, camouflaging irregularities and hiding the edges of underlying implants.
Nipples, too, can be reconstructed by folding skin into a cylindrical projection, and/or grafting the skin around it to simulate a textured areola. Another option is 3-D tattooing. Unfortunately, neither approach guarantees a return of “erogenous sensation, because removing the nipple severs its nerve endings,” says New York plastic surgeon Alexes Hazen, MD.